If you or someone you know is navigating the journey with ulcerative colitis (UC), there’s something hopeful on the horizon. It’s about the way new treatments are being developed, and it’s centered around what matters most: you.
What is Ulcerative Colitis?
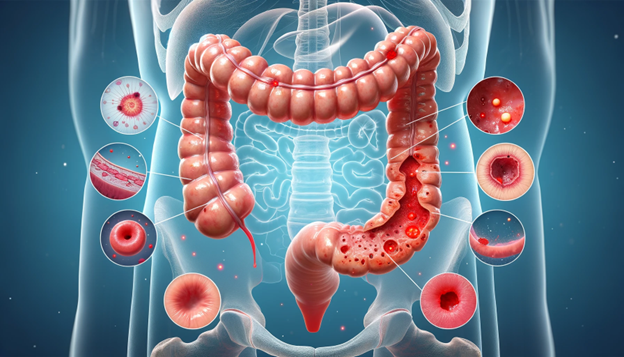
Ulcerative colitis is a chronic inflammatory bowel disease[1], a condition that causes inflammation and ulcers in the colon and rectum. It can lead to symptoms like stomach pain, urgent trips to the bathroom, and even blood in the stool. The incidence and regularity of UC have seen a steady rise over the recent years, marking a continual increase in its progression [2].Living with UC can be challenging, not just physically but also emotionally [3]. The symptoms can vary in severity and may evolve over time. Common symptoms can include:
- Abdominal Pain [4] and Cramping: Many people with UC experience varying degrees of abdominal discomfort and cramps, often related to bowel movements.
- Diarrhea: Frequent, urgent bowel movements are common, and diarrhea can range from mild to severe in UC patients.
- Blood in Stool [5]: One of the hallmark symptoms of UC is the presence of blood or pus in the stool, ranging from small amounts noticed on toilet tissue to significant amounts mixed with the stool.
- Urgency to Defecate: Individuals with UC often feel a strong, urgent need to have a bowel movement, which can be distressing and disruptive to daily life.
- Weight Loss [6]: Unintended weight loss can occur, often due to reduced appetite, increased intestinal loss of proteins or nutrients, and the body’s increased energy expenditure due to inflammation.
- Fatigue[7]: Persistent tiredness or fatigue is common, likely due to the body’s response to chronic inflammation, anemia, or nutrient deficiencies.
- Fever: In more severe cases, UC can cause a low-grade fever, especially during flare-ups of the disease.
- Anemia: Due to chronic blood loss, some people with UC may develop anemia, which can lead to further fatigue and weakness.
- Reduced Appetite[8]: Inflammation and abdominal discomfort can lead to decreased appetite and nutritional deficiencies.
It’s important to note that the severity and presence of these symptoms can vary widely among individuals. Some may experience mild symptoms, while others have more severe and frequent flare-ups. These flare-ups are typically characterized by a rapid and intense progression, evidenced by severe diarrhea and cramps, fever, leukocytosis, and abdominal swelling. The condition, known as fulminant disease, is more common in children than adults[9]. Around 15% of those affected experience symptoms so severe that hospital admission is necessary[10,11]. Because UC can affect more than just the gastrointestinal tract, it may also cause systemic symptoms such as joint pain, skin problems, and eye inflammation in more severe cases.
Understanding Clinical Trials: How Your Participation Makes a Difference
Clinical trials are fundamental components of medical research, meticulously designed to test new treatments, drugs, or medical devices in humans. These studies are critical for advancing medical knowledge and improving patient care.
- Phases of Clinical Trials[12]: Clinical trials are conducted in several phases to assess a new treatment’s safety, efficacy, side effects, and optimal dosages:
- Phase I: The treatment is tested on a small group of people to evaluate its safety and identify side effects.
- Phase II: Expand the study to more people to assess efficacy and further evaluate safety.
- Phase III: Involves a larger group of participants to confirm effectiveness, monitor side effects, compare it to commonly used treatments, and collect information that will allow the treatment to be used safely.
- Phase IV: This phase is conducted after a treatment is approved and marketed to gather information on the drug’s effect in various populations and any side effects associated with long-term use.
Participant Selection
Trials have specific criteria for who can participate, known as inclusion and exclusion criteria. These criteria can include factors like age, gender, the type and stage of a disease, previous treatment history, and other medical conditions.
Informed Consent
Before participating, individuals must undergo an informed consent process, ensuring they understand the trial’s purpose, procedures, risks, benefits, and rights as participants, including the right to withdraw at any time.
Blinding
To further reduce bias, some trials are “blinded,” meaning that participants (and sometimes the researchers) do not know who is receiving the experimental treatment and who is receiving a placebo or standard treatment.
Monitoring
Throughout the trial, participants are closely monitored for responses to the treatment and any side effects. This monitoring can provide valuable information on how the treatment impacts UC and the patient’s quality of life.
Results and Impact
After a trial is completed, researchers analyze the data to understand the treatment’s effectiveness and safety. The findings can lead to new treatment options for UC, influencing future care standards and potentially improving patient outcomes.
Your Role in Clinical Trials
Participating in a clinical trial can be a deeply personal decision that contributes significantly to medical research and the potential development of new UC treatments. Participants can gain access to new therapies, contribute to the scientific understanding of UC, and help future patients receive better care.
If you’re considering joining a clinical trial, discuss it with your healthcare provider to understand the potential benefits and risks, and how a specific trial might align with your health goals and needs.

How Are We Making UC Trials Better for Patients?
Historically, the success of clinical trials for conditions like UC was measured primarily through clinical endpoints, such as endoscopic findings and histological assessments. However, this approach often overlooked the patient’s perspective on their symptoms and the impact of the disease on their daily lives. Researchers and healthcare professionals have recognized this gap shifted towards a more holistic model emphasizing patient-reported outcomes (PROs).
The good news is that the way we test new UC treatments is changing for the better, focusing more on what patients really need and want. At the forefront of this patient-centric approach is the innovative design of clinical trials[13], which have increasingly begun to prioritize patient needs, preferences, and experiences. We prioritize this at FOMAT Medical Research, one of the largest clinical trial networks in California.

Listening to Your Voice
In the past, doctors and scientists mainly looked at medical tests to see if a treatment was working. But now, there’s a big push to listen to what you, the patient, are saying about your own health. This means paying attention to how you’re feeling overall, how much your symptoms are affecting your daily life, and what kind of side effects you might be experiencing from the treatment. This approach helps make sure that new treatments are not only effective but also make a real difference in patients’ lives.
Engaging with Patients: Beyond the Clinical Setting
Another critical evolution in UC trials is the emphasis on patient engagement. This approach involves patients in the trial design process, ensuring that studies are not only about them but also with them. Imagine being part of a group that gets to share ideas and feedback about what it’s like to live with UC and what you hope for in a treatment. This kind of input is invaluable. It helps design studies that are easier for patients to take part in and more focused on what truly matters to those living with UC.

FOMAT Medical Research: Leading with Compassion
Here at FOMAT Medical Research, we’re proud to be leading the way in these patient-centered UC trials. Our aim is to make sure that every study we conduct takes into account the real-world experiences and needs of UC patients like you. By fostering an environment of collaboration and empathy, we strive to advance scientific understanding and enhance the care and quality of life for individuals living with UC.
How Can You Get Involved?
We believe that together, we can make a real difference in the world of UC treatment. Whether you’re living with UC, caring for someone who is, or just interested in helping advance UC research, there’s a place for you here.
If you’re curious about our studies or thinking about joining one, we’d love to hear from you. Getting involved could not only help you but also pave the way for better treatments for others in the UC community.
Reach out to FOMAT Medical Research today to learn more or to get started.
Citations:
- Peng, S., Shen, L., Yu, X., Zhang, L., Xu, K., Xia, Y., Zha, L., Wu, J., & Luo, H. (2023). The role of Nrf2 in the pathogenesis and treatment of ulcerative colitis. Frontiers in Immunology, 14, 1200111. https://doi.org/10.3389/fimmu.2023.1200111
- Krugliak Cleveland, N., Torres, J., & Rubin, D. T. (2022). What does disease progression look like in ulcerative colitis, and how might it be prevented? Gastroenterology, 162(5), 1396–1408. https://doi.org/10.1053/j.gastro.2022.01.023
- Brydolf, M., & Segesten, K. (1996). Living with ulcerative colitis: Experiences of adolescents and young adults. Journal of Advanced Nursing, 23(1), 39–47. https://doi.org/10.1111/j.1365-2648.1996.tb03133.x
- Sinopoulou, V., Gordon, M., Dovey, T. M., & Akobeng, A. K. (2021). Interventions for the management of abdominal pain in ulcerative colitis. Cochrane Database of Systematic Reviews, (7), CD013589. https://doi.org/10.1002/14651858.CD013589.pub2
- Kornbluth, A., & Sachar, D. B. (2010). Ulcerative colitis practice guidelines in adults: American College of Gastroenterology, Practice Parameters Committee. The American Journal of Gastroenterology, 105(3), 501–523. https://doi.org/10.1038/ajg.2009.727
- Gajendran, M., Loganathan, P., Jimenez, G., Catinella, A. P., Ng, N., Umapathy, C., Ziade, N., & Hashash, J. G. (2019). A comprehensive review and update on ulcerative colitis. Disease-a-Month, 65(12), 100851. https://doi.org/10.1016/j.disamonth.2019.02.004
- Regueiro, M., Hunter, T., Lukanova, R., & others. (2023). Burden of fatigue among patients with ulcerative colitis and Crohn’s disease: Results from a global survey of patients and gastroenterologists. Advances in Therapy, 40, 474–488. https://doi.org/10.1007/s12325-022-02364-2
- Kucharzik, T., Koletzko, S., Kannengiesser, K., & Dignass, A. (2020). Ulcerative colitis-diagnostic and therapeutic algorithms. Deutsches Ärzteblatt International, 117(33-34), 564–574. https://doi.org/10.3238/arztebl.2020.0564
- Falcone RA Jr, Lewis LG, Warner BW. Predicting the need for colectomy in pediatric patients with ulcerative colitis. J Gastrointest Surg. 2000 Mar-Apr;4(2):201-6. doi: 10.1016/s1091-255x(00)80057-8. PMID: 10675244.
- Rowe FA, Walker JH, Karp LC, Vasiliauskas EA, Plevy SE, Targan SR. Factors predictive of response to cyclosporin treatment for severe, steroid-resistant ulcerative colitis. Am J Gastroenterol. 2000 Aug;95(8):2000-8. doi: 10.1111/j.1572-0241.2000.02186.x. PMID: 10950049.
- Rowe FA, Walker JH, Karp LC, Vasiliauskas EA, Plevy SE, Targan SR. Factors predictive of response to cyclosporin treatment for severe, steroid-resistant ulcerative colitis. Am J Gastroenterol. 2000 Aug;95(8):2000-8. doi: 10.1111/j.1572-0241.2000.02186.x. PMID: 10950049.
- Friedman, L. M., Furberg, C. D., DeMets, D. L., Reboussin, D. M., & Granger, C. B. (2015). Fundamentals of clinical trials. Springer.
- Alsoud, D., Verstockt, B., Fiocchi, C., & Vermeire, S. (2021). Breaking the therapeutic ceiling in drug development in ulcerative colitis. The Lancet Gastroenterology & Hepatology, 6(7), 589–595. https://doi.org/10.1016/s2468-1253(21)00065-0

